Apolipoprotein A1 and B Most Popular
- $220.80
- $55.95
- Save: 74.66%
The following is a list of what is included in the item above. Click the test(s) below to view what biomarkers are measured along with an explanation of what the biomarker is measuring.
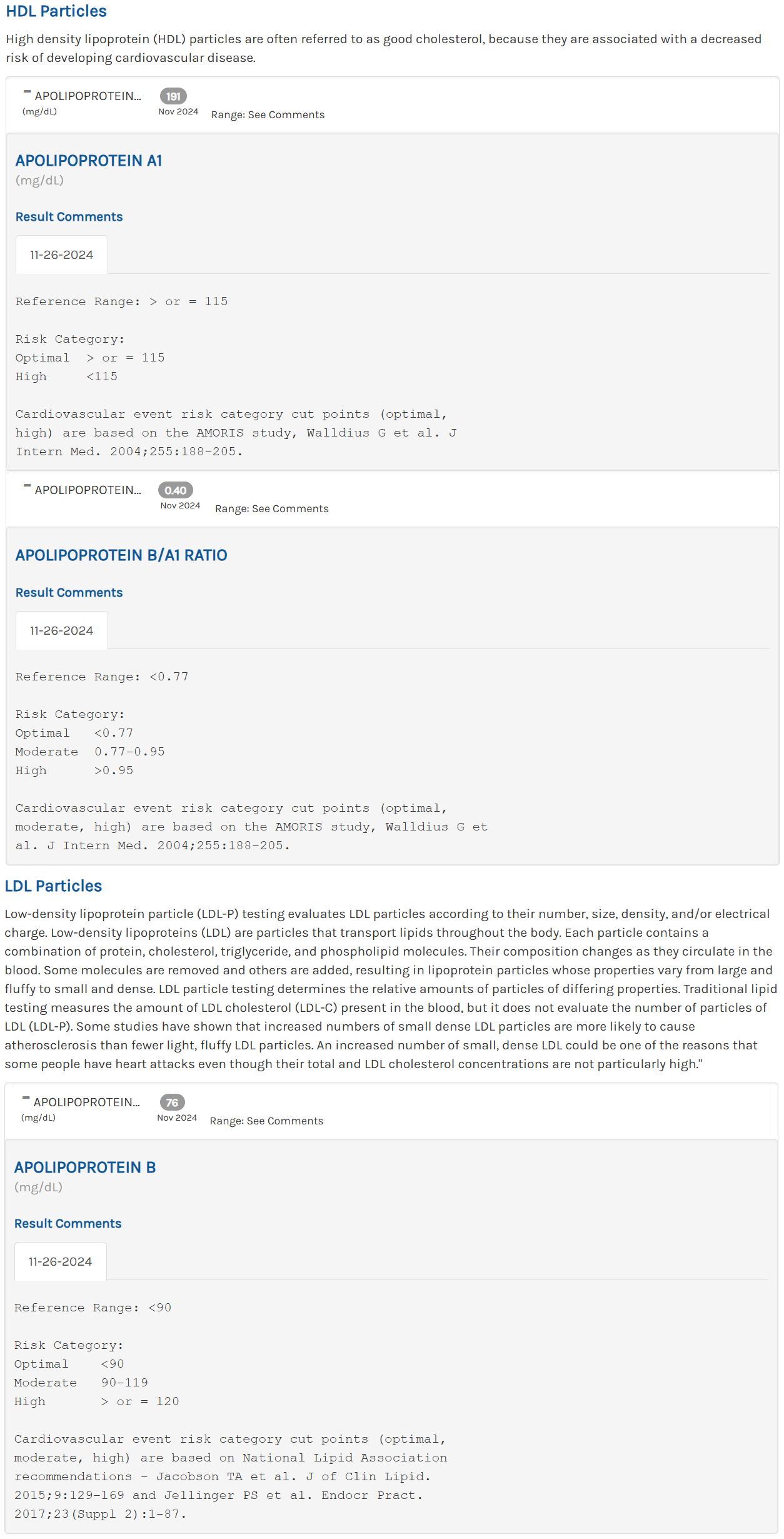
Apolipoprotein A1
Apolipoprotein B
Apolipoprotein B/A1 Ratio
The Apolipoprotein A1 and B test contains 1 test with 3 biomarkers .
Brief Description: The Apolipoprotein A1 and B test is a laboratory test that measures the levels of two important proteins, apolipoprotein A1 (apo A1) and apolipoprotein B (apo B), in the blood. These proteins are essential components of lipoproteins, which transport cholesterol and triglycerides in the bloodstream.
Also Known As: Apo A1 and B Test, Apolipoprotein Evaluation Test
Testing Method: Immunoturbidimetric
Collection Method: Blood Draw ![]()
Specimen: 1 mL Serum 
Test Preparation: Fasting for 12 hours is required.
When are Apolipoprotein A1 and B tests ordered?
An Apolipoprotein A1 and B test may be ordered in the following situations:
-
Cardiovascular Risk Assessment: The test is commonly ordered to assess an individual's risk of developing cardiovascular diseases, such as coronary artery disease (CAD), atherosclerosis, or heart attack. Apo A1 and apo B levels provide valuable information about lipoprotein metabolism and cholesterol transport, which are key factors in cardiovascular health.
-
Monitoring Lipid Disorders: The test is useful in monitoring individuals with known lipid disorders, including high cholesterol (hypercholesterolemia) or low HDL cholesterol levels (HDL-C), to evaluate the effectiveness of treatment and assess the risk of cardiovascular complications.
-
Evaluation of Lipoprotein Abnormalities: An Apolipoprotein A1 and B test can help identify specific lipoprotein abnormalities, such as high levels of small, dense LDL particles or low levels of protective HDL particles. These abnormalities contribute to an increased risk of cardiovascular diseases.
What does Apolipoprotein A1 and B blood tests check for?
Lipids are transported throughout the bloodstream by apolipoproteins, which mix with them. Lipoproteins are held together by apolipoproteins, which protect the water-repellent lipids at their core.
Lipoproteins are cholesterol or triglyceride-rich proteins that transport lipids throughout the body for cell absorption. HDL, on the other hand, is like an empty cab or taxi. It travels to the tissues to collect excess cholesterol before returning it to the liver. Cholesterol is either recycled for future use or eliminated in bile in the liver. The only mechanism for cells to get rid of excess cholesterol is by HDL reverse transport. It protects the arteries and, if enough HDL is present, it can even reverse the formation of fatty plaques, which are deposits caused by atherosclerosis and can contribute to cardiovascular disease.
Sticking with the taxi analogy, the driver is Apolipoprotein A. It permits HDL to be detected and bound by receptors in the liver at the end of the transport by activating the enzymes that load cholesterol from the tissues into HDL. Apolipoprotein A is divided into two types: apo A-I and apo A-II. Apo A-I has a higher prevalence than apo A-II. Apo A-I concentrations can be evaluated directly, and they tend to rise and fall in tandem with HDL levels. Deficiencies in apo A-I are linked to an increased risk of cardiovascular disease.
Chylomicrons are lipoprotein particles that transport dietary fats from the digestive system to tissue, primarily the liver, via the bloodstream. These dietary lipids are repackaged in the liver and combined with apo B-100 to create triglyceride-rich VLDL. This combo is similar to a taxi with a full load of passengers and apo B-100 as the driver. The taxi moves from place to place in the bloodstream, releasing one passenger at a time.
Triglycerides are removed from VLDL by an enzyme called lipoprotein lipase, which produces intermediate density lipoproteins first, then LDL. VLDL contains one molecule of apo B-100, which is kept as VLDL loses triglycerides and shrinks to become the cholesterol-rich LDL. Apo B-100 is detected by receptors on the surface of many different types of cells in the body. The absorption of cholesterol into cells is aided by these receptors.
LDL and apo B-100 transport cholesterol that is essential for cell membrane integrity, sex hormone generation, and steroid production. Excess LDL, on the other hand, can cause fatty deposits in artery walls, as well as blood vessel hardening and scarring. Atherosclerosis is a condition in which fatty deposits restrict blood arteries. The risk of a heart attack increases as the atherosclerotic process progresses.
LDL-C levels, which are typically ordered as part of a lipid profile, tend to mimic Apo B-100 levels. Many experts believe that apo B levels will eventually show to be a more accurate predictor of CVD risk than LDL-C. Others disagree, believing that apolipoprotein B is only a modestly superior choice and that it should not be used on a regular basis. The clinical utility of apo B, as well as other developing cardiac risk markers including apo A-I, Lp(a), and hs-CRP, is still unknown.

Lab tests often ordered with Apolipoprotein A1 and B tests:
When an ApoA1 and ApoB test is ordered, it's often part of a broader assessment of cardiovascular risk. Here are some tests commonly ordered alongside it:
-
- Purpose: Measures total cholesterol, HDL cholesterol, LDL cholesterol, and triglycerides.
- Why Is It Ordered: To provide a basic overview of lipid levels. The standard lipid panel is a primary tool for assessing cardiovascular risk and guides treatment decisions.
-
- Purpose: Measures the level of Lp(a), a type of lipoprotein associated with an increased risk of cardiovascular disease.
- Why Is It Ordered: Lp(a) is a genetically determined risk factor for cardiovascular disease and can provide additional risk assessment, especially in individuals with a family history of heart disease.
-
High-Sensitivity C-Reactive Protein (hs-CRP):
- Purpose: A marker of inflammation in the body.
- Why Is It Ordered: Inflammation plays a significant role in atherosclerosis and cardiovascular disease. Elevated hs-CRP levels are associated with an increased risk of heart attacks and strokes.
-
Fasting Blood Glucose and Hemoglobin A1c (HbA1c):
- Purpose: Measures blood sugar control and diabetes risk.
- Why Is It Ordered: Diabetes is a significant risk factor for cardiovascular disease. These tests help identify diabetes or prediabetes, which require management to reduce cardiovascular risk.
-
Thyroid Function Tests (TSH, Free T3, Free T4):
- Purpose: To assess thyroid function.
- Why Is It Ordered: Thyroid disorders can affect lipid metabolism, influencing cholesterol levels and cardiovascular risk.
-
- Purpose: To evaluate kidney function.
- Why Is It Ordered: Kidney disease can impact cardiovascular health and lipid metabolism.
These tests, when ordered alongside an ApoA1 and ApoB test, provide a comprehensive view of an individual’s risk factors for cardiovascular disease. They help in identifying underlying conditions that may contribute to cardiovascular risk and guide treatment and lifestyle interventions to mitigate these risks. The selection of these tests will depend on the individual's overall health, family history of cardiovascular disease, and existing risk factors.
Conditions where Apolipoprotein A1 and B tests are recommended:
The Apolipoprotein A1 and B test is particularly relevant for individuals with the following conditions or diseases:
-
Cardiovascular Diseases: Individuals with a family history of premature cardiovascular diseases, personal history of heart disease, or risk factors like hypertension, diabetes, or obesity may require an Apolipoprotein A1 and B test to assess their cardiovascular risk.
-
Dyslipidemia: Individuals with abnormal lipid profiles, including high LDL cholesterol, low HDL cholesterol, or high triglyceride levels, may undergo an Apolipoprotein A1 and B test to provide a more detailed assessment of their lipoprotein profile.
-
Monitoring Lipid-Lowering Therapy: Patients undergoing lipid-lowering treatment, such as statin medications, may have their Apolipoprotein A1 and B levels monitored to evaluate the effectiveness of therapy and adjust treatment plans if necessary.
How does my healthcare provider use Apolipoprotein A1 and B tests?
Health care providers use the results of an Apolipoprotein A1 and B test to:
-
Assess Cardiovascular Risk: By analyzing the ratio of apo B to apo A1, along with other lipid parameters, health care providers can determine an individual's cardiovascular risk and develop appropriate prevention and treatment strategies.
-
Guide Treatment Decisions: The test results help guide treatment decisions for lipid disorders. For example, if an individual has elevated apo B levels or an unfavorable apo B to apo A1 ratio, aggressive lipid-lowering therapies or lifestyle modifications may be recommended to reduce the risk of cardiovascular events.
-
Monitor Treatment Response: Serial measurements of Apolipoprotein A1 and B levels allow health care providers to monitor the effectiveness of lipid-lowering interventions, such as medication and lifestyle modifications, and make necessary adjustments to achieve target levels and reduce the risk of cardiovascular complications.
It's important to note that the interpretation of Apolipoprotein A1 and B test results should be done in the context of the individual's overall health, medical history, and other risk factors to guide personalized treatment plans and preventive strategies.
What do my Apolipoprotein A1 and B test results mean?
Low apo A-I levels are linked to low HDL levels and slowed elimination of excess cholesterol from the body. Low levels of apo A-I, as well as high levels of apo B, are linked to a higher risk of cardiovascular disease.
Deficiencies in apo A-I are caused by a number of hereditary diseases. Abnormal lipid levels, notably excessive amounts of low-density lipoprotein, are common in people with certain illnesses. They frequently have a higher rate of atherosclerosis. Low apo A-I levels are caused by several genetic diseases.
Raised apo B levels are linked to elevated LDL-C and non-HDL-C levels, and are linked to an increased risk of cardiovascular disease. Elevations may be caused by a high-fat diet and/or a reduction in LDL clearance from the blood.
A direct cause of abnormal apo B levels is some hereditary diseases. Familial combined hyperlipidemia, for example, is an inherited condition that causes excessive cholesterol and triglyceride levels in the blood. Apolipoprotein B deficiency, also known as Bassen-Kornzweig syndrome, is a relatively rare hereditary disorder that results in unusually low amounts of apo B.
A variety of underlying diseases and other factors might result in abnormal apo B levels.
Most Common Questions About the Apolipoprotein A1 and B test:
Understanding the Apolipoprotein A1 and B Test and Its Purpose
What is the Apolipoprotein A1 and B test?
The Apolipoprotein A1 and B test is a blood test that measures the levels of two proteins, Apolipoprotein A1 (Apo-A1) and Apolipoprotein B (Apo-B), which are key components of lipoproteins that transport cholesterol and triglycerides in the blood.
Why would a doctor order an Apolipoprotein A1 and B test?
A doctor might order this test if they need more information about a patient's risk of developing cardiovascular disease, beyond what's provided by a standard lipid profile. These apolipoproteins are associated with "good" (HDL) and "bad" (LDL) cholesterol respectively, and their levels can offer additional insights into heart health.
Who might need an Apolipoprotein A1 and B test?
This test might be recommended for individuals who have a personal or family history of heart disease or if they have other risk factors such as smoking, high blood pressure, diabetes, or obesity.
Interpreting Test Results and Abnormal Findings
What do the results of an Apolipoprotein A1 and B test mean?
A high level of Apo-A1 (associated with HDL, or "good" cholesterol) is generally desirable and indicates a lower risk of cardiovascular disease. A high level of Apo-B (associated with LDL, or "bad" cholesterol) could suggest an increased risk of cardiovascular disease.
What does a high Apolipoprotein A1 test result indicate?
A high Apolipoprotein A1 level is generally a positive sign, as Apo-A1 is a component of HDL, the "good" cholesterol. Higher levels of HDL and therefore Apo-A1 are associated with a lower risk of heart disease.
What does a high Apolipoprotein B test result mean?
A high Apolipoprotein B level could indicate a higher risk of cardiovascular disease. Apo-B is a component of LDL, the "bad" cholesterol, and higher levels are associated with an increased risk of plaque buildup in the arteries.
How are the results of an Apolipoprotein A1 and B test used in combination with other tests?
The results of this test are often used in combination with other tests such as a lipid panel, which measures total cholesterol, HDL, LDL, and triglycerides. The ratio of Apo-B to Apo-A1 can also provide valuable insights into a patient's cardiovascular risk.
Understanding the Implications and Health Impact
What role do Apolipoprotein A1 and B play in the body?
Apolipoprotein A1 and B are proteins that bind to lipids (fats) to form lipoproteins, which transport cholesterol and triglycerides in the blood. Apo-A1 is a major component of HDL, or "good" cholesterol, and helps remove cholesterol from the body. Apo-B is a major component of LDL, or "bad" cholesterol, and delivers cholesterol to tissues.
What health conditions can be associated with abnormal Apolipoprotein A1 and B levels?
Abnormal levels of these apolipoproteins can be associated with an increased risk of cardiovascular disease, including heart disease and stroke. High levels of Apo-B or low levels of Apo-A1 might indicate an increased risk of plaque buildup in the arteries.
Risk Factors, Prevention, and Treatment
What factors might influence my Apolipoprotein A1 and B levels?
Various factors can influence these levels, including diet, exercise, weight, genetics, age, sex, and the presence of other health conditions like diabetes or hypothyroidism. Certain medications can also affect these levels.
How can I maintain or improve my Apolipoprotein A1 and B levels?
Maintaining a healthy lifestyle is key. This includes eating a balanced diet low in saturated fats and cholesterol, exercising regularly, maintaining a healthy weight, avoiding smoking, and managing stress. Medications can also be used to manage these levels if necessary.
What treatment options exist for abnormal Apolipoprotein A1 and B levels?
Treatment will depend on the underlying cause. Lifestyle changes are usually the first line of treatment, but medications like statins or other lipid-lowering drugs may be prescribed if necessary. It's important to discuss treatment options with a healthcare provider.
Keywords: Apo A1 Test, Apo B Test, APOAB Test, Apolipoprotein B-100 Test,
